Does the Sex of the Surgeon Influence Long-Term Surgical Outcomes in Female and Male Patients?
Key Highlights
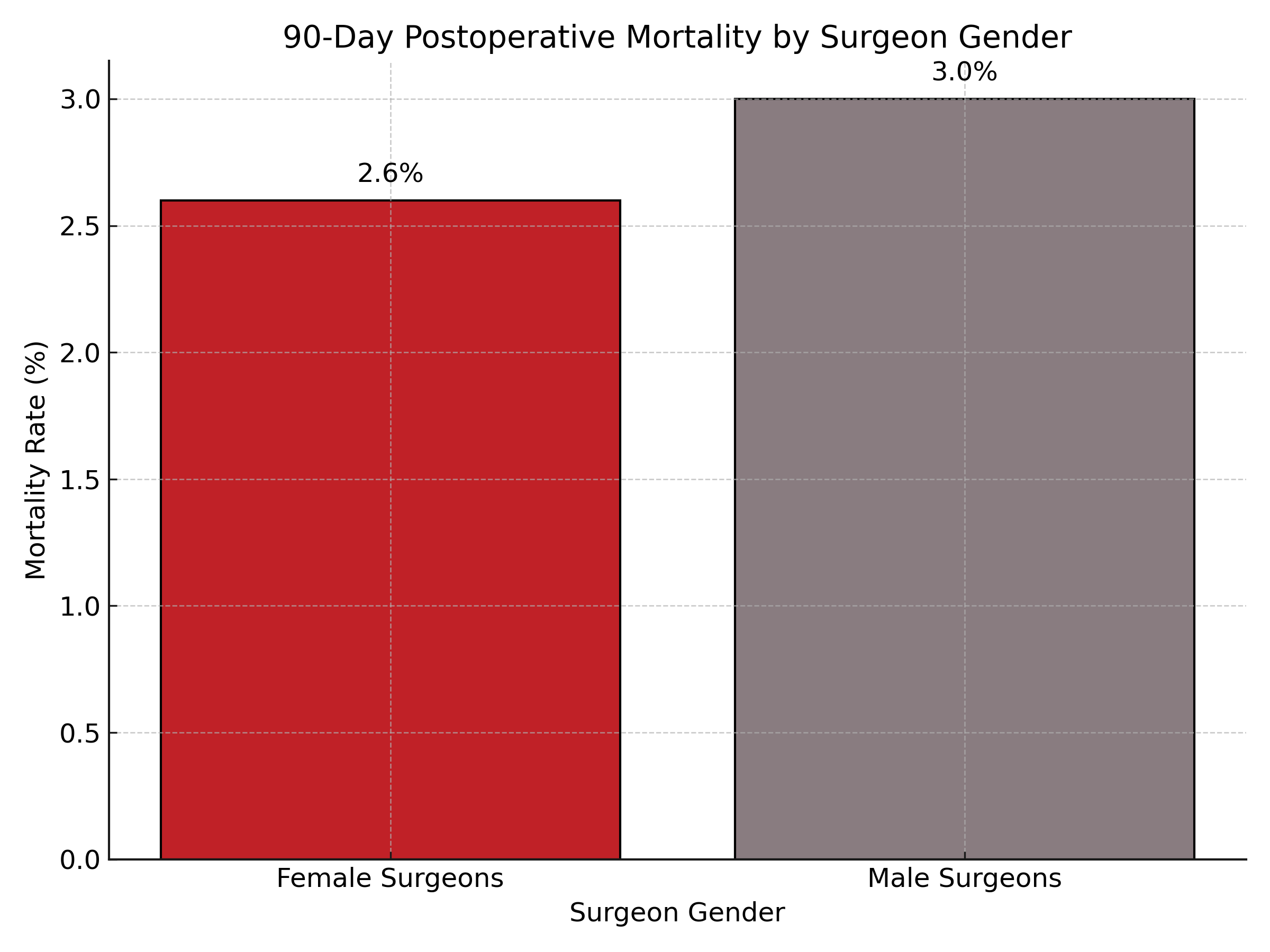
- Female surgeons had lower long-term mortality rates than male surgeons for both female and male patients.
- Female patients treated by female surgeons experienced fewer readmissions and complications.
- Gender concordance benefited only female patients in terms of long-term postoperative outcomes.
- No significant differences in outcomes were observed for male patients based on surgeon gender.
In a large cross-sectional study of more than 2.2 million Medicare beneficiaries undergoing one of 14 major surgeries, patients of either sex treated by female surgeons experienced better long-term outcomes than those treated by male surgeons. Most notably, female patients who were treated by female surgeons had significantly lower rates of readmissions and complications in the 90 days following surgery. These benefits were not observed in male patients, whose outcomes did not differ by the surgeon’s gender.
Research into how physician and patient characteristics affect clinical outcomes has grown in recent years. While existing evidence suggests physician gender and gender concordance may improve outcomes—especially for female patients—there has been limited study of this relationship in the context of long-term surgical outcomes in the United States. This study addresses that gap by examining whether outcomes differ depending on the gender of the surgeon and whether there is a match between the gender of the patient and the surgeon.
Investigators conducted a population-based cross-sectional study using 100% Medicare fee-for-service claims data from 2016 through 2019. Eligible participants were Medicare beneficiaries aged 65 to 99 who underwent one of 14 elective or emergent surgical procedures in acute care hospitals across the United States. Data analysis, completed in early 2025, compared 90-day and 1-year postoperative mortality, readmission, and complication rates by surgeon gender and patient-surgeon gender concordance. Analyses adjusted for both patient and surgeon characteristics and used hospital fixed effects to ensure comparability across settings.
Of the 2,288,279 patients included, only 5.7% were treated by female surgeons. Nonetheless, female surgeons were associated with better long-term outcomes. Adjusted 90-day mortality rates were lower for patients treated by female surgeons (2.6%) compared with male surgeons (3.0%), with similar benefits observed in both female and male patients. Among female patients specifically, gender concordance with a female surgeon resulted in reduced 90-day readmission rates (7.3% vs 7.7%) and complication rates (12.2% vs 12.8%). No such differences were found among male patients based on gender concordance. These outcome patterns were consistent at both the 90-day and 1-year time points.
“In this study, both female and male patients treated by female surgeons experienced lower long-term postoperative mortality rates compared with those treated by male surgeons,” the study authors concluded. “Patient-surgeon gender concordance was associated with lower long-term readmission and complication rates for female patients, but not for male patients.”
Reference:
Ikesu R, Gotanda H, Russell TA, et al. Long-term postoperative outcomes by surgeon gender and patient-surgeon gender concordance in the US. JAMA Surg. 2025;160(6):624-632. doi:10.1001/jamasurg.2025.0866


