Peer Reviewed
Bell Palsy as an Atypical Presenting Symptom of Type 2 Diabetes Mellitus
Authors:
Eric Sales, MD; Kathryn Tierling, MD; Angela S. Byrd, MD; and Emily L. Klepper, MD
Our Lady of the Lake Children’s Hospital and Pediatric Residency Program, Baton Rouge, Louisiana
Citation:
Sales E, Tierling K, Byrd AS, Klepper EL. Bell palsy as an atypical presenting symptom of type 2 diabetes mellitus [published online August 28, 2018]. Neurology Consultant.
An obese 14-year-old boy presented to the emergency department (ED) with a 2-day history of left cheek pain and drooping of the left side of his face. He also reported a 2- to 3-month history of polyuria, polydipsia, and a 15.4-kg weight loss. At presentation, he had mild altered mental status with slowed mentation.
Physical examination. The patient was afebrile (temperature, 37°C) and had a heart rate of 97 beats/min, a respiratory rate of 14 breaths/min, blood pressure of 126/98 mm Hg, and a body mass index of 31 kg/m2. He had an asymmetric smile with left-sided drooping, an inability to puff out the left cheek, and left eye ptosis. He also had loss of forehead and eyebrow movement of the left side. Neck examination revealed hyperpigmentation of the posterior neck consistent with acanthosis nigricans.
Cardiac examination revealed normal S1 and S2 with no murmurs, gallops, or rubs. The lung fields were clear to auscultation bilaterally with no rales, rhonchi, or wheezing. The abdomen was soft, nontender, and nondistended, with normal bowel sounds. Sensation was intact throughout, with normal motor function in all extremities.
Diagnostic tests. Laboratory test results obtained in the ED were significant for a blood glucose level of 569 mg/dL; urinalysis revealed a glucose level greater than 1000 mg/dL and a ketone level of 20 mg/dL. Results of a complete blood cell count with differential and venous blood gas testing were within normal limits. Results of a comprehensive metabolic panel showed a blood glucose level of 761 mg/dL and an anion gap of 12 mEq/L. The glycated hemoglobin concentration was elevated at 17.1%.
Based on his clinical presentation and diagnostic test results, the patient received a diagnosis of new-onset diabetes mellitus without diabetic ketoacidosis and Bell palsy (idiopathic peripheral nerve palsy).
Treatment. The patient was given a normal saline bolus and was started on insulin glargine, 40 U daily at bedtime; insulin lispro, 1 U for every 10 g of carbohydrates consumed with meals and snacks; and a sliding-scale correction of 1 U of insulin lispro for every 40 mg/dL above a blood glucose level of 160 mg/dL.
Further workup to differentiate type 1 diabetes mellitus (T1DM) vs type 2 diabetes mellitus (T2DM) included assays for immunoglobulin A antibodies, tissue transglutaminase antibodies, glutamic acid decarboxylase antibodies, complement-fixing islet cell autoantibodies, and islet cell immunoglobulin G autoantibodies, the results of which all were normal, confirming the diagnosis of T2DM. Corticosteroids were not given due to their potential to induce further hyperglycemia. Acyclovir was not started, since there was no clear indication that a prior viral infection had precipitated the facial palsy. Diabetes management was continued with the addition of metformin, 1000 mg twice daily.
Discussion. Approximately 12 in 100,000 US children and adolescents have T2DM,1,2 and the incidence is increasing. African Americans, Hispanics, Asian/Pacific Islanders and American Indians are at increased risk of developing T2DM.1,3
Most children with T2DM are obese and can present with polyuria, polydipsia, glucosuria, hypertension, dyslipidemia, acanthosis nigricans, and/or metabolic syndrome.1,4 Facial nerve palsy, however, is not part of the typical T2DM presentation in children and appears 2 to 4 times less frequently in children than in adults.5,6
Bell palsy is an acute, often idiopathic, lower motor neuron peripheral palsy of cranial nerve VII. It accounts for approximately 40% to 70% of facial nerve palsy cases (Figures 1 and 2). The estimated annual incidence of Bell palsy is 6.1 cases per 100,000 in individuals between 1 and 15 years of age.7,8
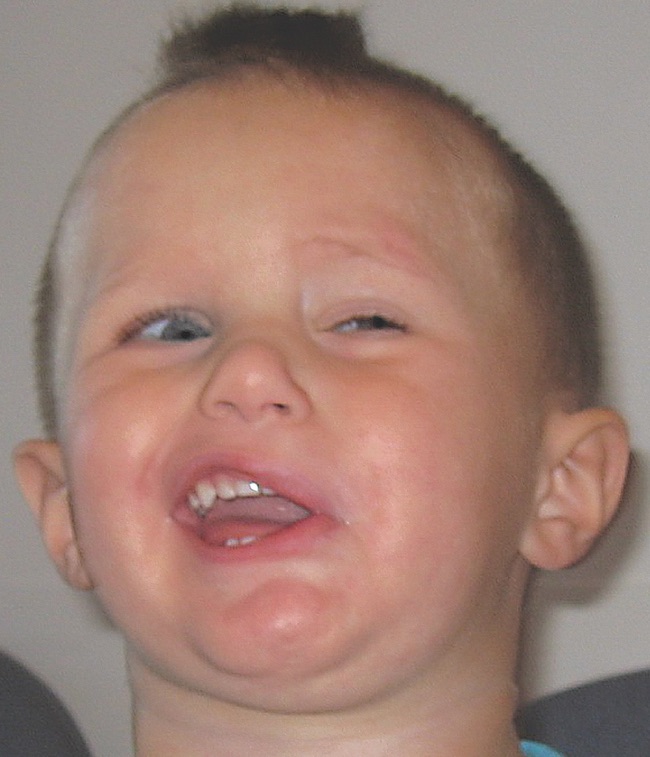
Figure 1. Bell palsy in a 22-month-old boy. From: Janjua HS, Ayoob R, Spencer JD. Hypertension in a boy with Bell palsy. Consultant for Pediatricians. 2011;10(6):203-206.

Figure 2. Bell palsy in a 7-year-old girl. From: Tadphale S, Butterfield R. What is the cause of this child’s facial asymmetry? Consultant for Pediatricians. 2012;11(1):III.
Research in the adult population with diabetes shows a correlation between poor glycemic control and the development of Bell palsy. The more elevated the glycated hemoglobin level, the more severe the facial nerve palsy.9 While age is a major risk factor for developing Bell palsy, diabetes has also been identified as an independent risk factor that is present in more than 10% of adults with Bell palsy.10,11
Short-term improvements in glycemic control have been shown to have a restorative effect in facial nerve palsy, and glycemic control can prevent facial nerve palsy in adult patients with diabetes.9
To date, only 1 other published case report has identified an adolescent with Bell palsy and concurrent new-onset diabetes.12 The patient was treated with corticosteroids and metformin, and the authors hypothesized that the known relationship between diabetes and Bell palsy in adults could extend to the pediatric population. However, treatment with corticosteroids in all children with Bell palsy remains controversial. A randomized controlled study in children with Bell palsy found a recovery rate of 80% to 90% in the first 6 months and 100% by 1 year irrespective of treatment with corticosteroids.13 Facial nerve palsy outcomes appear to be more favorable in children compared with adults, with almost complete recovery within 6 months.6,14 Corticosteroid-induced hyperglycemia further supports avoiding corticosteroid treatment in persons with diabetes and Bell palsy.
Outcome of the case. The patient’s facial nerve palsy improved dramatically as his blood glucose level returned to normal. Prior to discharge on hospital day 3, he was able to puff out his cheeks, close his mouth, close his eyes, speak without stuttering or drooling, and smile with only slight facial asymmetry.
- Reinehr T. Type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2013;4(6):270-28
- Liese AD, D’Agostino RB Jr, Hamman RF, et al; SEARCH for Diabetes in Youth Study Group. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118(4):1510-1518.
- Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136(5):664-672.
- Rosenbloom AL, Silverstein JH, Amemiya S, Zeitler P, Klingensmith GJ. ISPAD clinical practice consensus guidelines 2006–2007: type 2 diabetes mellitus in the child and adolescent. Pediatr Diabetes. 2008;9(5):512-526.
- El-Hawrani AS, Eng CY, Ahmed SK, Clarke J, Dhiwakar M. General practitioners’ referral pattern for children with acute facial paralysis. J Laryngol Otol. 2005;119(7):540-542.
- Finsterer J. Management of peripheral facial nerve palsy. Eur Arch Otorhinolaryngol. 2008;265(7):743-752.
- Özkale Y, Erol İ, Saygı S, Yılmaz İ. Overview of pediatric peripheral facial nerve paralysis: analysis of 40 patients. J Child Neurol. 2015;30(2):193-199.
- Barr JS, Katz KA, Hazen A. Surgical management of facial nerve paralysis in the pediatric population. J Pediatr Surg. 2011;46(11):2168-2176.
- Riga M, Kefalidis G, Danielides V. The role of diabetes mellitus in the clinical presentation and prognosis of Bell palsy. J Am Board Fam Med. 2012;25(6):819-826.
- Monini S, Lazzarino AI, Iacolucci C, Buffoni A, Barbara M. Epidemiology of Bell’s palsy in an Italian health district: incidence and case-control study. Acta Otorhinolaryngol Ital. 2010;30(4):198-204.
- Pecket P, Schattner A. Concurrent Bell’s palsy and diabetes mellitus: a diabetic mononeuropathy? J Neurol Neurosurg Psychiatry. 1982;45(7):652-655.
- Kim TS, Cho WK, Cho KS, et al. A case of type 2 diabetes mellitus in adolescent presenting with Bell’s palsy. Ann Pediatr Endocrinol Metab. 2012;17(4):258-261.
- Marenda SA, Olsson JE. The evaluation of facial paralysis. Otolaryngol Clin North Am. 1997;30(5):669-682.
- Ashtekar CS, Joishy M, Joshi R. Do we need to give steroids in children with Bell’s palsy? Emerg Med J. 2005;22(7):505-507.


