Burkitt Lymphoma
Authors:
Christopher K. Kitterman, DO, and Alberto Marante, MD
Department of Pediatrics, PBCGME/Palms West Children’s Hospital, Loxahatchee, Florida
Andrew C. Berry, DO
Department of Medicine, University of South Alabama, Mobile, Alabama
Citation:
Kitterman CK, Marante A, Berry AC. Burkitt lymphoma [published online November 16, 2017]. Consultant360.
An 8-year-old boy with a history of asthma presented to the emergency department with a chief concern of a sore throat of 1 week’s duration. The patient had right-sided face and neck swelling and a fever, with a maximum temperature of 38.9°C. The mother reported that the boy had had halitosis and a 5.4-kg weight loss in the past 2 months.
On physical examination, the patient’s blood pressure was 120/70 mm Hg, his heart rate was 105 beats/min, his respiratory rate was 22 breaths/min, and his temperature was 37.0°C. The patient weighed 35 kg, was awake and alert, was obese, had right-sided facial swelling, and spoke with a hoarse voice. The posterior pharynx had right-sided swelling and purulent drainage.
Laboratory tests revealed a white blood cell count of 15,700/µL, a hemoglobin level of 13.9 g/dL, and a platelet count of 416 × 103/µL. Serum chemistry test results were within normal limits. The C-reactive protein level was 0.7 mg/L, and the lactate dehydrogenase (LDH) level was 213 U/L.
Neck computed tomography (CT) showed a soft-tissue mass in the right peritonsillar area measuring 2.7 × 2.2 cm. The patient was admitted to the pediatric intensive care unit for close monitoring and concern for airway deterioration. An otorhinolaryngologist was consulted.
The patient was treated for atypical peritonsillar abscess with intravenous (IV) clindamycin, cefuroxime, and dexamethasone. After 2 days of IV antibiotics had led to no improvement, a direct rigid bronchoscopy was performed. The results yielded a large exophytic, friable soft-tissue mass, grossly consistent with tumor, involving the right tonsillar region with displacement of the uvula to the left. A biopsy specimen of the mass was obtained. The patient remained intubated to protect his airway and was started on mechanical ventilation.
Flow cytometry of the biopsy sample showed immunophenotypic evidence of a CD10+ clonal B-cell population, a finding consistent with a B-cell lymphoma. Biopsy results were positive for MYC rearrangement and additional copies of IGH and had a starry-sky appearance consistent with Burkitt lymphoma (Figures 1-3).
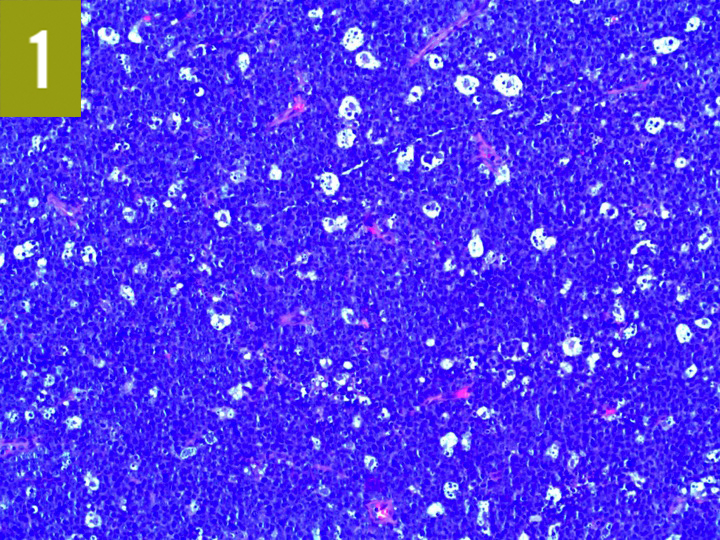
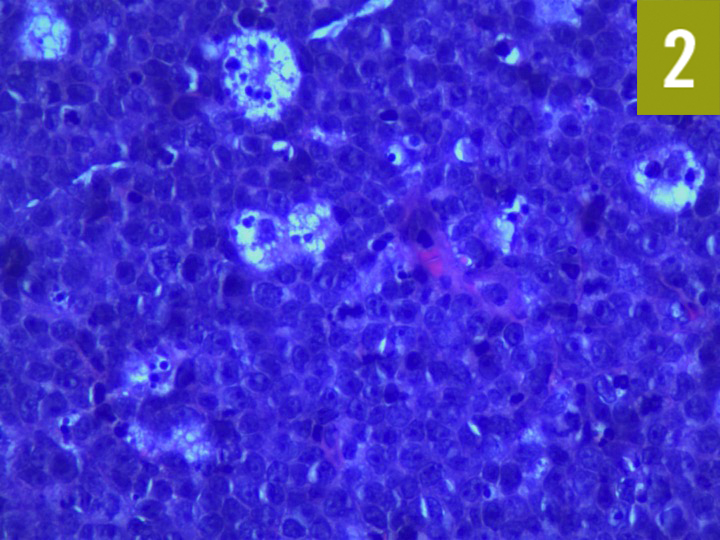
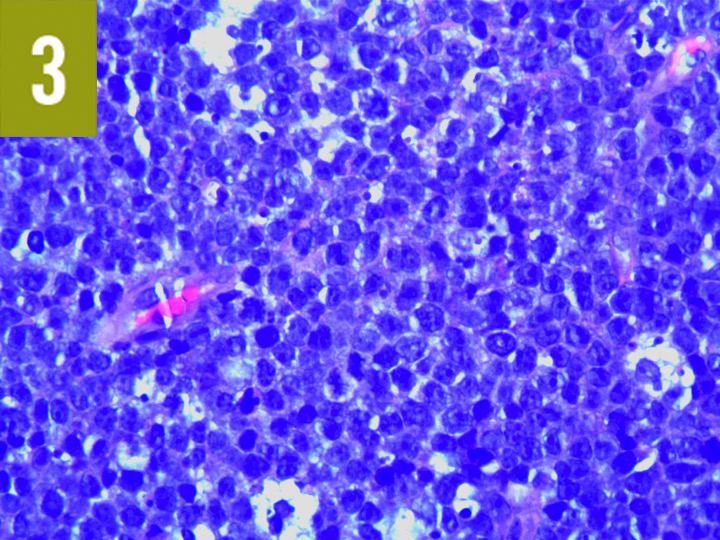
Figures 1-3: Tumor cells are large, with minimal cytoplasm, and form a dark blue “sky” appearance. Tingible body macrophages consume cellular debris that appears as large white “stars.”
The patient was begun on induction therapy with cyclophosphamide, vincristine, and prednisolone per the Children’s Oncology Group Burkitt lymphoma protocol ANHL01P1. CT images of the neck 8 days after chemotherapy induction showed 100% resolution of the bilateral tonsil masses and a substantial interval reduction of 50% in bilateral cervical lymphadenopathy.
Discussion
Burkitt lymphoma is an aggressive B-cell non-Hodgkin lymphoma characterized by the translocation of MYC on chromosome 8. The 3 types of Burkitt lymphoma are endemic or African (most often characterized by jaw involvement), sporadic or non-African (most often intra-abdominal), and immunodeficiency-associated.1
Symptoms include weight loss, fever, and night sweats (ie, B symptoms), as well as fatigue, joint pain, pharyngitis, pruritus, ascites, hepatosplenomegaly, and intussusception. Two major epidemiologic risk factors are malaria and Epstein-Barr virus infection, both of which cause B-cell hyperplasia due to MYC translocation.2
Abnormal laboratory test findings include anemia, thrombocytopenia, leukopenia, hyperuricemia, acute kidney failure, and an elevated LDH level. Burkitt lymphoma carries a potential for tumor lysis syndrome, leading to the release of large amounts of potassium, phosphate, and uric acid, causing acute renal failure. Histologically, Burkitt lymphoma has a starry-sky appearance due to medium-size lymphoid cells with high proliferative and apoptotic activity.3
Immunohistochemical analysis reveals B-cell differentiation (CD20, CD22, CD19, CD10, BCL6) with high mitotic activity cells staining positive for Ki-67. The most common variant (85%-90% of cases) is t(8;14) translocation of MYC and IGH.
Chemotherapy protocols include cyclophosphamide, doxorubicin, vincristine, methotrexate, cytarabine, ifosfamide, etoposide, and rituximab. Staging can be performed by way of CT, positron-emission tomography, lumbar puncture, or bone marrow aspiration and biopsy.
The prognosis is excellent, with a greater than 90% survival rate for stages I and II and 80% to 90% for stages III and IV. The prognosis can be affected by incomplete remission, an elevated LDH level, advance-stage disease, and delay in treatment.5
The early diagnosis of Burkitt lymphoma is important if a patient has enlarged supraclavicular lymph nodes, lymph nodes increasing in size over 2 weeks, constitutional symptoms, or enlarged lymph nodes over 6 weeks. The differential diagnosis of a sore throat must remain broad, especially in the clinical context of other symptoms such as fever and weight loss. It is imperative to closely monitor patients presenting with these symptoms to determine when further workup is necessary.
References:
- Hecht JL, Aster JC. Molecular biology of Burkitt’s lymphoma. J Clin Oncol. 2000;18(21):3707-3721.
- Magrath I. Epidemiology: clues to the pathogenesis of Burkitt lymphoma. Br J Haematol. 2012;156(6):744-756.
- Swerdlow SH, Campo E, Harris NL, et al, eds. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon, France: International Agency for Research on Cancer Press; 2008. WHO Classification of Tumours; vol 2.
- Fujita S, Buziba N, Kumatori A, Senba M, Yamaguchi A, Toriyama K. Early stage of Epstein-Barr virus lytic infection leading to the “starry sky” pattern formation in endemic Burkitt lymphoma. Arch Pathol Lab Med. 2004;128(5):549-552.
- Cairo MS, Sposto R, Gerrard M, et al. Advanced stage, increased lactate dehydrogenase, and primary site, but not adolescent age (≥ 15 years), are associated with an increased risk of treatment failure in children and adolescents with mature B-cell non-Hodgkin’s lymphoma: results of the FAB LMB 96 study. J Clin Oncol. 2012;30(4):387-393.


