A Case of Multiple Brain Metastases with an Unknown Primary Malignancy
Case Presentation
Mrs. C is a 67-year-old African-American woman who presented to an outpatient clinic with a several-week history of episodic aphasia, confusion, and left-sided paresthesias. A previous outpatient evaluation conducted at the onset of her symptoms had included a computed tomography (CT) scan of the brain without contrast, which was negative for any abnormality. At that time, a transient ischemic attack was diagnosed, and the patient was placed on aspirin 81 mg daily. Mrs. C’s neurological symptoms resolved temporarily, only to return the following week. Her confusion worsened, so she presented to the outpatient clinic for evaluation. Her review of systems was positive for mild anorexia, decreased taste sensation, and a 15-lb weight loss over the past month.
The patient’s medical history was notable for hypertension and a cerebrovascular accident in 2001, from which she had no neurological sequalea. She reported a, she had a chronic cough in 2007 for which she underwent a pulmonary evaluation in another state, including a CT scan of the chest. The cough resolved after a prolonged course of antibiotics, and she had no subsequent follow-up; her physicians at the outpatient clinic were unable to obtain records of that evaluation. Mrs. C’s only chronic medications were lisinopril 20 mg daily and aspirin. Her smoking history was positive for 1 pack per day for 40 years. She rarely drank alcohol and took no recreational drugs.
The physical examination revealed a fatigued-appearing, elderly African-American woman who appeared older than her stated age and who was in no acute distress. Her vital signs were within normal limits. The patient was alert and oriented x 4. The head, eyes, ears, nose, and throat examination was unremarkable. The neck examination was negative for masses and elevated jugular venous pressure. Her lungs were clear to auscultation throughout. The cardiovascular examination showed a regular heart rate and rhythm without murmurs. Her speech was clear, and her gag reflex was intact. The neurological examination showed normal facial symmetry and intact sensation to light touch throughout her facial muscles. Mrs. C’s pupils were equal and reactive to light bilaterally, and her visual fields were full. Her extraocular muscles were intact bilaterally, her motor strength was 5/5 throughout, and her coordination was intact with finger to nose bilaterally. The patient’s reflexes were slightly greater in the right lower extremity as compared with the left. Toes were downgoing bilaterally. Complete blood cell count, electrolyte levels, and liver function tests were all within normal limits. The chest x-ray was clear of infiltrates, but showed a nodular mass in the left apical region. A non-contrast CT scan of the head was repeated and was negative for any acute abnormalities. Because of her persistent symptoms, a magnetic resonance imaging (MRI) scan of the brain with contrast was 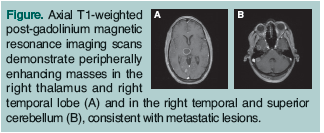 obtained; several masses were identified (Figure). The patient then underwent percutaneous fine needle aspiration of the left apical mass, which revealed small cell carcinoma.
obtained; several masses were identified (Figure). The patient then underwent percutaneous fine needle aspiration of the left apical mass, which revealed small cell carcinoma.
Discussion
Brain metastases account for over half of all intracranial tumors in adults, with carcinomas being the most common type. In the majority of cases, patients who are diagnosed with brain metastases have an established diagnosis of a primary malignancy (metachronous presentation). Metastases can be diagnosed simultaneously with the primary tumor (synchronous presentation) or, as in the case discussed in this article, before the underlying malignancy is identified (precocious presentation). In decreasing order, the incidence of brain metastases detected in each of the following types of cancer has been reported as follows: lung (16%-20%); renal cell (7%-10%); melanoma (7%); breast (5%); and colorectal (1%-2%).1,2 Hematogenous spread is thought to be the likely route in which metastases reach the brain.3 Brain metastases are responsible for a wide range of clinical presentations, including aphasia, headache, cognitive/memory dysfunction, and seizures.
Brain metastases are discovered on imaging studies, with contrast-enhanced MRI being the most sensitive modality available. Ample evidence establishes the increased sensitivity of contrast-enhanced MRI over MRI without contrast and CT scans in detecting brain lesions, and in detecting metastatic brain lesions in particular. Characteristics that have been found to be helpful in distinguishing metastatic lesions from primary brain tumors include multiple lesions, location of lesions at watershed areas, and increased vasogenic edema relative to size.4 Multiple newer modalities are under investigation, including echo planar imaging, spectroscopy, and single photon emission computed tomography (SPECT); however, their widespread role in the diagnostic approach to brain lesions has yet to be elucidated.
An initial evaluation of a patient presenting with possible brain metastases includes a thorough history (with attention to recent cancer screening and smoking history, in particular) and a detailed physical examination. Given the high likelihood of the lung as a primary source, a chest x-ray is essential; however, given the lack of sensitivity of chest x-rays, a chest CT scan should also be strongly considered, especially in patients with a smoking history or with other known risk factors for lung cancer. A CT scan of the abdomen and pelvis and a bone scan are usually also warranted and can assess for evidence of the primary tumor, if still unknown, or can help assess the extent of metastatic disease.
Biopsies for confirmation are typically performed on the lesions that are discovered after the initial evaluation. In situations where primary malignancy is undiagnosed after a thorough evaluation or where primary brain tumors are more likely (single lesions), biopsy of the intracranial lesions is warranted.
Treatment is generally divided into the acute management of the side effects of the brain lesions, prevention of complications, and systemic treatment of the underlying malignancy. Systemic treatment has generally been guided by the prognosis of the patient.5 In patients with a poor prognosis (widespread metastatic disease, age > 75 years, poor functional status, significant neurological dysfunction), acute symptom control, typically with steroids, and supportive care are the mainstays of therapy. Whole brain radiation therapy (WBRT) has been shown to be effective at improving neurological symptoms and decreasing lesion size.6,7 Patients with a relatively favorable prognosis whose conditions have certain specific characteristics (single lesions in accessible areas of the brain, good functional status) are potential candidates for neurosurgical resection. Stereotactic radiosurgery (SRS) is an option in patients with more than one lesion, an inaccessible single lesion, or lesions that are not otherwise amenable to resection. WBRT is commonly used in conjunction with neurosurgical resection and SRS to reduce the size of the lesions and recurrence rate.8, 9
Outcome of the Case Patient
The patient received WBRT with initial improvement of her symptoms over the course of several weeks after her small cell carcinoma was diagnosed. Her cognitive dysfunction slowly returned, and her family decided to pursue palliative measures only. Mrs. C died approximately 5 months after her initial presentation to the outpatient clinic.
The authors report no relevant financial relationships.
Dr. McElhannon is Associate Residency Director, and Dr. Muneer is Resident Physician, Atlanta Medical Center Family Medicine Residency, Morrow, GA.
References
1. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 2004;22(14):2865-2872.
2. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 2002; 94(10):2698-2705.
3. Arnold SM, Patchell RA. Diagnosis and management of brain metastases. Hematol Oncol Clin North Am 2001;15(6):1085-1107, vii.
4. Loeffler JS, Patchell RA, Sawaya R. Metastatic brain cancer. In: Devita VT, Hellman S, Rosenberg SA, eds. Cancer: Principles and Practice of Oncology. Philadelphia, PA: Lippincott Williams Wilkins; 1997:2523.
5. Gasper L, Scott C, Rotman M, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997;37(4):745-751.
6. Cairncross JG, Kim JH, Posner JB. Radiation therapy for brain metastases. Ann Neurol 1980;7(6):529-541.
7. Nieder C, Berberich W, Schnabel K. Tumor-related prognostic factors for remission of brain metastases after radiotherapy. Int J Radiat Oncol Biol Phys 1997;39(1):25-30.
8. Mintz A, Perry J, Spithoff K, Chambers A, Laperriere N. Management of single brain metastases: A practice guideline. Curr Oncol 2007;14(4):131-143.
9. Mehta MP, Tsao MN, Whelan TJ, et al. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 2005;63(1):37-46.


